On March 16, 2024, at Massachusetts General Hospital, for the first time in history, Harvard Medical School physician-scientists successfully transplanted a genetically edited pig kidney into a human patient in a groundbreaking medical procedure. This milestone achievement, conducted on 62-year-old Richard Slayman, holds significant promise for addressing critical shortages of human kidneys for patients with end-stage kidney failure, and it marks a major advancement in the field of xenotransplantation—the transplantation of organs or tissues from other animals into humans.
Slayman, who suffers from end-stage kidney disease, had previously received a human kidney transplant in 2018 that failed after 5 years of use, requiring him to return to dialysis. Dialysis is a medical procedure that helps perform the functions of a healthy kidney by filtering waste, removing excess fluids, and balancing electrolytes in the body. It is a tedious and challenging process because it requires regular sessions and is associated with physical discomfort. An article by CNN published Slayman’s thoughts on the surgery from a written statement provided by the hospital: “I saw [xenotransplantation] not only as a way to help me, but a way to provide hope for the thousands of people who need a transplant to survive.”
His surgery is the third instance of transplanting a pig organ into a living human. Surgeons at the University of Maryland operated on the first two cases, which involved heart transplants for individuals who had exhausted all other transplant options. Although the organs functioned and were not immediately rejected, both patients passed away within weeks of receiving the transplants. According to Dr. Winfred Williams, Slayman’s primary nephrologist, taking the risk of organ rejection was worth it: “He would have had to wait five to six years for a human kidney. He would not have been able to survive it.”The success of Slayman’s transplant is attributed to years of collaborative research by thousands of scientists and physicians. According to Harvard Medical School, the pig kidney used in the surgery was genetically modified by eGenesis using CRISPR-Cas9 gene-editing technology to remove certain pig genes that produce sugars that human immune systems will reject, add human genes to improve compatibility, and inactivate retroviruses present in pig genomes to eliminate the risk of infection.
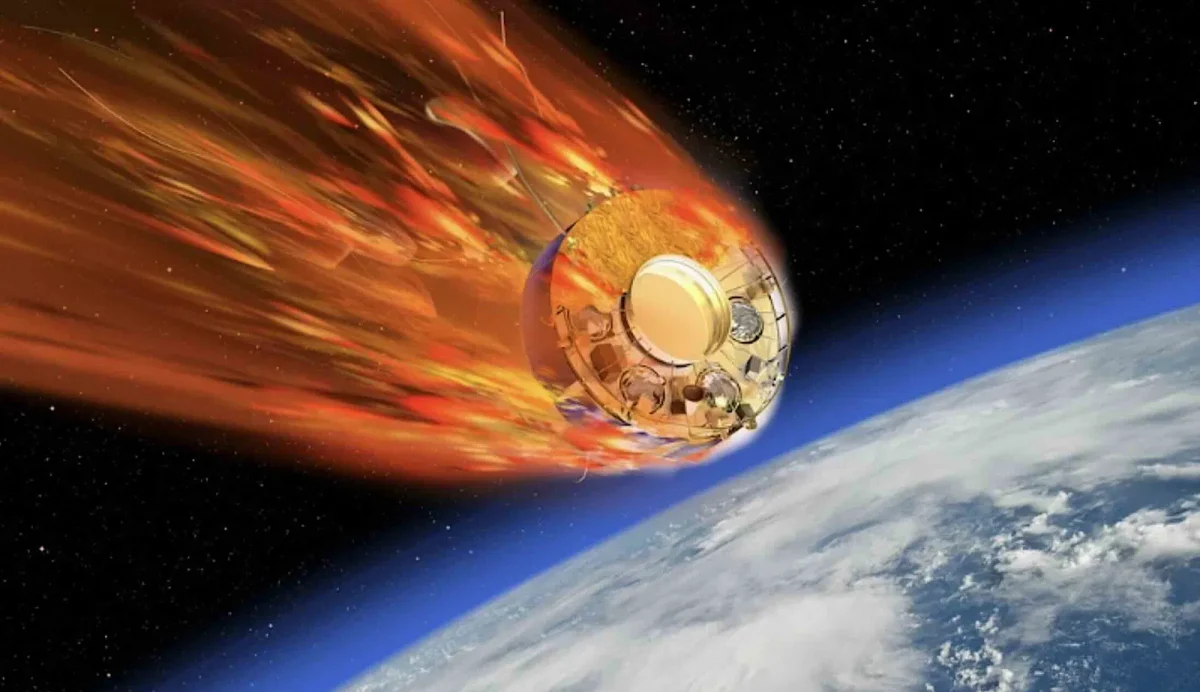
The surgery, which lasted four hours, was led by Dr. Tatsuo Kawai, Dr. Nahel Elias, and Dr. Leonardo Riella. Shortly after the pig kidney was stitched in and connected to Slayman’s blood vessels, the kidney began producing urine, indicating immediate function. Applause emerged from the 15-member transplant team in the operating room, who continued to diligently observe him to ensure a safe recovery.
Furthermore, this procedure holds special hope for Black patients who suffer from high frequencies of end-stage kidney disease. As a man of color, Slayman is commended for courageously accepting the risks of xenotransplantation to provide hope for the thousands of people anxiously waiting for a miracle. Whether it is accessibility to medical facilities or treatment affordability, minority patients face disparities in healthcare, which is why Slayman’s pig transplant holds such important value not only medically but also economically and socially.
It’s hard to imagine that pigs could be the key to revolutionizing organ transplantation and advancing medical science. While pigs have been the primary focus for xenotransplantation research, because of their physiological similarities and genetic compatibility with humans, other animals including primates (baboons), non-human primates (monkeys), and rodents (rats and mice) have also been experimented with. Although the long-term results of the transplant are not yet clear, Dr. Kawai is hopeful, according to an article by Harvard Medical School: “We still don’t know how many years this kidney can survive, but based on our preclinical research, we are aiming at years — more than two years.” Ultimately, this pioneering surgery offers hope for millions of patients worldwide suffering from organ failure. The success of this procedure could potentially reduce the need for dialysis and increase the availability of organs for transplantation, saving lives and improving the quality of life for patients in need.